SPA Meeting Reviews
Friday Session IV: There is a Fracture, Must We Fix It? An Orthopedics Refresher
Reviewed by Sean Flack, MBChB, FCA
Seattle Children’s Hospital
Sabina DiCindio, DO (Nemours/Alfred I. DuPont Hospital for Children) began the session with a talk titled “Little People and Anesthesia: Lessons Learned in the Last 25 Years” that addressed the anesthetic implications of skeletal dysplasias such as achondroplasia, Osteogenesis Imperfecta, Metatropic Dysplasia and Morquio’s Syndrome. Skeletal Dysplasias are generalized abnormalities of the skeleton involving bones and cartilage. Disproportionate short stature is a common feature and more than 400 SDs have been identified with an incidence of 1:5000 live births. In response to case reports of neurologic misadventure, Dr. Di Cindio advised caution with positioning (prone in particular) of these patients. Regional anesthesia has been safely performed without major complications, however further study is warranted.
In a recent retrospective study of Osteogenesis Imperfecta (OI) patients, NIBP cuffs and tourniquets were not associated with iatrogenic fractures and no complications from intra-arterial catheter use was found.
The anesthetic challenges that present in children with OI are nicely represented in this chart and greatest in severe OI (Type III):
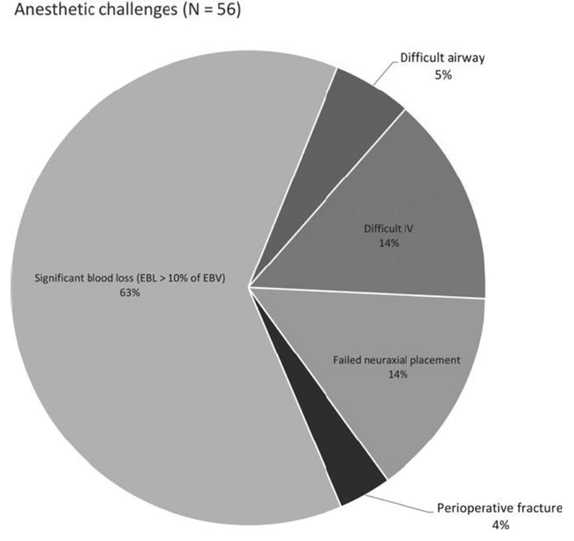
Rothschild L et al. Paediatr Anaesth. 2018; 28:1050-1058
Meatropic Dysplasia is an autosomal dominant condition with unknown incidence. Airway management is often challenging in these patients, particularly if spinal fusion has been performed. Morquio Syndrome is autosomal recessive with a 1:200 000 incidence and both upper and lower airway abnormalities are seen in these children. Tracheal narrowing, buckling and twisting is common, worsens with age and may be improved with surgical reconstruction. Importantly, neuraxial anesthesia must be avoided in these patients and careful attention paid to positioning and spinal cord perfusion.
David Martin, MD (Nationwide Children’s Hospital) followed with a talk titled “New Regional Blocks: Suprascapular, Suprainguinal Fascia Iliaca, and Superficial Cervical Plexus”. Suprascapular nerve block is useful as an adjunct to arthroscopic shoulder surgery without risk for phrenic nerve palsy. If performed, consider adding an axillary nerve block for better coverage. Beware of accidental arterial injection (use color doppler). Superficial cervical plexus blocks are indicated for clavicular fractures, repairs, internal jugular vein cannulation, carotid endarterectomy and other procedures involving the lateral neck, posterior ear and anterior shoulder. It is a fascial plane block with potential for causing phrenic nerve block. Ultrasound guided suprainguinal Fascia Iliaca blocks have been shown to successfully anesthetize the femoral and lateral femoral cutaneous nerves and may be a more reliable technique than the traditional infra-inguinal approach.
“Squiggles, Wiggles, and Drugs: Anesthesia and Pediatric Intraoperative Neuromonitoring” was the title of the next lecture by Michael Puglia, MD, PhD (University of Michigan). We make clinical decisions based on inferences drawn from values that we monitor. Evoked potentials are a surrogate measure for perfusion of the spinal cord. A limitation in pediatric anesthesia is the energy needed to elicit adequate signals. Kids need increased voltage and motor evoked potentials (MEPs) are the most difficult to elicit. Nevertheless, neuromonitoring is important in the prevention of injury as new neurological deficits occur in 1.4% of children following scoliosis surgery. A 50% decrease in somatosensory evoked potentials (SSEPs) or 100% for MEPs is the threshold for poor outcomes. SSEP amplitude has been shown to decrease over time with isoflurane compared to propofol. MEP response significantly increased when sevoflurane anesthesia was switched to propofol. Ketamine has been shown to increase cortical responses at low to moderate doses. However, dexmedetomidine decreases MEP amplitude and should be used with caution and in low doses. Opioids do not affect signals.
Dr. Puglia recommended propofol, low dose ketamine and an opioid of choice as the preferred anesthetic for patients requiring neuromonitoring. Other important variable to consider include temperature, blood pressure, ventilation and hematocrit. Good communication between surgeon, anesthesiologist and neuromonitoring technician is vital.
The final talk in this session was by Jim Mooney, MD (Children’s Healthcare of Atlanta) who spoke on the topic “Intrathecal Morphine vs. Methadone for Major Orthopedic Surgery”. This is a topic that has generated a lot of interest and increasing numbers of publications in recent years. Methadone has been around for a long time but remains an “easy” option due to its pharmacology (onset time similar to fentanyl; long half-life). Intrathecal morphine gained interest after 2000. Pain relief appeared to be better than methadone but at the expense of side-effects (pruritus, urinary retention and respiratory depression).
Subsequent studies may allow us to draw the following conclusions about intravenous methadone versus intrathecal morphine: Perioperative methadone use results in less respiratory events, is better for neuropathic pain and easier to administer. Intrathecal morphine is associated with reduced bleeding.
Dr. Mooney concluded that cultural comfort and flexibility on the part of surgical nursing staff may determine which option is best in your institution.